What is Babesia (Babesiosis )
What is Babesia?
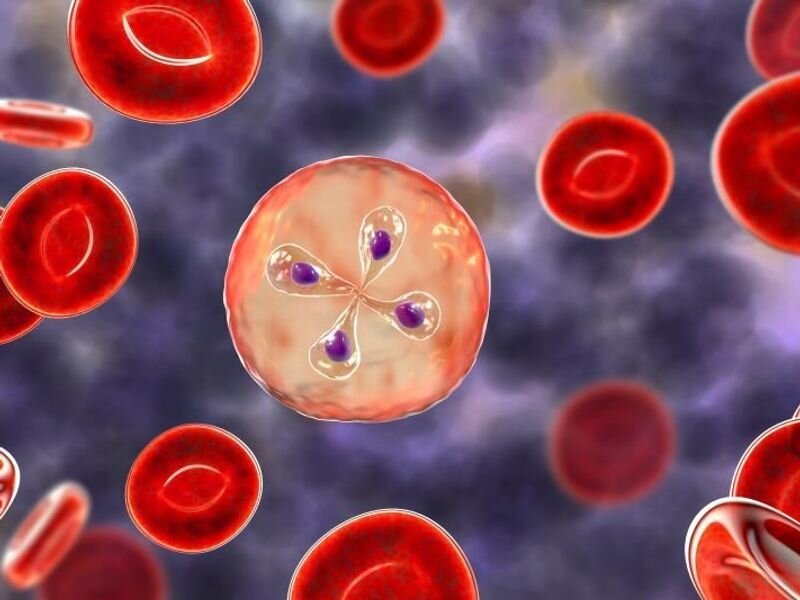
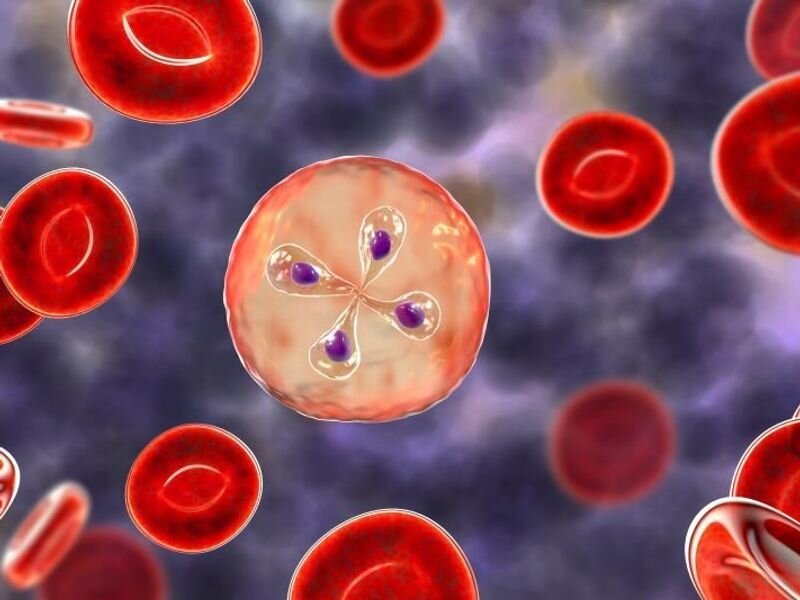
What is Babesiosis? More commonly known as Babesia is a malaria-like protozoal parasite that infects red blood cells. It is primarily spread by the bite of the deer tick, Ixodes scapularis. As this paper acknowledges, Babesia is a growing public health issue that deserves more attention and necessitates the need for better screening methods for blood donors.
Babesia can also be acquired via:
Bite by an infected vector (such as a tick)
Babesiosis is considered one of the most common Lyme co-infections.
In a survey conducted by LymeDisease.org, over half of the 3,000 participating chronic Lyme disease patients reported having at least one other infection. Of all co-infections, Babesiosis was diagnosed in 32% of responders.
In another survey conducted in Canada, at least one coinfection was reported by 60% of responders with Babesiosis affecting around 30%.
It is evident from these surveys that all Lyme patients should also be tested for Babesiosis and other co-infections.
While Babesia microti is believed to cause the majority of human illness, other species such as Babesia divergens and Babesia duncani have also been reported. It is important to note that because some tests only detect a single species, false negatives can occur if the patient is infected with a species for which the test is not meant to detect
Symptoms of Babesiosis infection are:
Drenching sweats during the day or night
Fever
Shortness of breath/air hunger
Fatigue and body aches
Headache
Pain in the muscles and joints
Gastrointestinal symptoms (nausea, abdominal pain, diarrhea)
Skin rashes (rare)
Severe symptoms can include:
Jaundice (yellowing of the skin and eyes)
Petechiae (pinpoint bruises under the skin)
Dark urine
Pulmonary edema (fluid in the lungs)
Symptoms can last weeks to months, and relapses that cycle every few months is not unusual.
How is Babesiosis diagnosed?
Diagnosis of Babesia infection is not straightforward and can be difficult.
The least technical test is direct visualization. In this test, the patient’s blood is examined under a microscope using a blood smear and a common laboratory stain. The stain provides contrast between the blood cells and the parasite and can enhance visualization, but it is not specifically designed to detect Babesia. For this reason, and because there are typically low numbers of Babesia in the blood, the direct visualization testing method often results in false negatives.
One method uses a molecular technique called Polymerase Chain Reaction, or PCR. This test can detect even a small amount of Babesia DNA in a blood sample.
Fluorescent In-Situ Hybridization assay, or FISH test is another test option. Like the direct visualization method, a blood smear from the patient is prepared. However, with the FISH method, the smear is treated with a special fluorescent stain that is specifically designed to attach to Babesia. When the blood smear is examined under a microscope, the Babesia can literally be seen glowing inside the red blood cell. Because this test is specific for a single species of Babesia, it will not cross-react with other species and can lead to a false negative result if a less common species is present. For example, a FISH test for B. macroti will not detect B. duncani and vice versa.
Because of the difficulties and complexities involved in diagnosis, it is recommended that a combination of testing methods be used.
A more complete discussion of testing methods and their limitations is available through IGeneX Inc., one of the most respected tick-borne illness testing laboratories.
Summary:
Babesiosis is a relatively common Lyme co-infection with up to one-third of Lyme patients affected.
Symptoms vary widely and can include air hunger, joint pain, headaches, fatigue, and general malaise. In some instances, Babesia can manifest as a severe, acute infection requiring aggressive treatment, or it can become a more chronic, low-grade infection that tends to wax and wane. Diagnosis of Babesia can be difficult as testing methods are not fool-proof and false negatives can occur. Diagnosis and subsequent treatment are best performed by a Lyme Literate Medical Doctor (LLMD) to ensure the most up-to-date treatment. A multi-pronged treatment approach involving pharmaceutical and non-pharmaceutical therapies is often used. Babesia is considered an emerging tick-borne illness that can often be chronic in nature. There is no known cure.
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
This page may contain affiliate links.
Are you searching for targeted support? This comprehensive formula is a synergistic blend of Samento (Uncaria tomentosa) bark, Stevia (Stevia rebaudiana) leaf, and Banderilla (Otoba parvifolia) bark, designed to assist with microbial support, immune system support, and healthy inflammatory response support.
FAQs about Babesiosis
-
Babesia is a type of microscopic parasite that infects red blood cells in humans and animals. It is commonly transmitted through tick bites, specifically by ticks of the genus Ixodes, which can also transmit Lyme disease.
-
Babesia infection can cause a range of symptoms, which may vary in severity. Common symptoms include:
Fever and chills.
Fatigue and weakness.
Headaches.
Muscle aches and joint pain.
Sweating.
Nausea and loss of appetite.
Shortness of breath.
Jaundice (yellowing of the skin and eyes) in severe cases.
-
Diagnosis of Babesia infection is typically done through a combination of clinical evaluation, medical history, and laboratory tests. Blood tests, such as a peripheral blood smear or PCR (polymerase chain reaction) test, can help detect the presence of Babesia parasites or their genetic material in the blood.
-
Yes, Babesia infection can be treated. The primary treatment for Babesia is a course of antiparasitic medications, such as atovaquone combined with azithromycin or clindamycin. The specific treatment regimen and duration may vary depending on the severity of the infection and individual factors. It is important to consult with a healthcare professional for proper diagnosis and appropriate treatment.Yes, Babesia infection can be treated. The primary treatment for Babesia is a course of antiparasitic medications, such as atovaquone combined with azithromycin or clindamycin. The specific treatment regimen and duration may vary depending on the severity of the infection and individual factors. It is important to consult with a healthcare professional for proper diagnosis and appropriate treatment.
-
Babesia is primarily transmitted through the bite of infected ticks. However, there have been rare cases of Babesia transmission through blood transfusions and organ transplants from infected donors. It is important to screen blood donations for Babesia to reduce the risk of transfusion-transmitted infections.
-
Babesia infection can lead to complications, especially in individuals with weakened immune systems, the elderly, or those with underlying health conditions. Possible complications include severe hemolytic anemia (breakdown of red blood cells), organ failure, and even death in rare cases.
-
To reduce the risk of Babesia infection, it is important to take preventive measures against tick bites, such as:
Wearing long-sleeved shirts, long pants, and closed-toe shoes when in tick-prone areas.
Conducting regular tick checks on yourself, family members, and pets after outdoor activities.
Creating tick-safe zones around your home by removing leaf piles and keeping lawns well-maintained.
Considering appropriate tick repellents and preventive treatments for pets.
-
Babesia infections occur in various parts of the world, but the prevalence may vary in different geographic regions. However, it's important to note that tick populations and infection rates can change over time, so staying informed about local tick-borne diseases is crucial.
-
Babesia infection can sometimes become chronic or recurrent, especially in individuals with weakened immune systems or those with persistent tick exposure. Chronic or recurrent Babesia infection may require extended treatments.



